ARCHIVES
Potential Briefs
ISSUE #06 — June 2012
Comment on this Newsletter... CLICK HERE
ANNOUNCEMENTS
Test your Knowledge!
For those of you who have read and internalized the Neurotechnologist Reference Guide, now you can check your level of understanding by taking one of the five online quizzes. Click on the following link to assess your knowledge today with a quiz on "Additional Recording Sites and Other Procedures from pages P68-129 in the Neurotechnologist Reference Guide.
Click here to test your knowledge
ARTICLE HIGHLIGHT
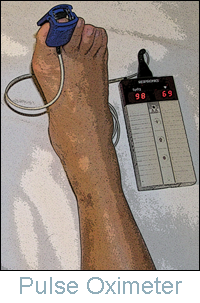
Article: Lower Extremity Pulse Oximetry for Anterior Lumbar Procedures
Authors: Ken S. Sato, MD, Daniel Slepian, PA, CNIM, Douglas Enoch, M.D., MSc, FACS.
Study Design: Retrospective Review
Introduction: The anterior approach is widely used for stabilization/decompression of the lumbar spine. This approach involves manipulation of the arteries overlying the spine, which can lead to vascular compromise. While intraoperative tibial somatosensory evoked potential has been used to detect this compromise the addition of intraoperative pulse oximetry of the left great toe provides a more rapid warning of limb ischemia.
Methods: An unselected series of 34 anterior lumbar procedures were monitored between October 1998 and August 2000. Tibial somatosensory evoked potentials (SSEPs) were recorded in all 34 procedures. A Nicolet Biomedical System (Bravo) was used to record intraoperative SSEPs from subdermal electrodes inserted after induction and positioning. Tibial nerves were simulated posterior to the medial malleolus at 2.7-4.7 Hz and 35mA and recorded from needle electrodes placed at the C7-T1 interspinous space, sagittal and parietal scalp, (Fpz-Cz), (Fpz-C3', C4'). Continuous stimulation with multiple repetitions was averaged with alteration between both legs. Oxygen saturation was monitored in addition to SSEPs in 11 procedures. A digital oxygen saturation monitor was attached to a left toe and measurements were recorded throughout the procedure. Serial blood pressures, core temperatures and anesthetic variations were also recorded throughout the procedure.
Results: Of the 23 procedures without oxygen saturation monitoring nine cases had significant (increased latency of 10% and/or an amplitude reduction of at least 50%) changes in the left tibial SSEPs, representing 26%. In all nine of these cases only the left tibial SSEP showed a significant change from baseline. The surgeon was immediately notified when a significant change occurred. In one case the left SSEP was completely obliterated while the right tibial SSEP showed no significant latency or amplitude abnormality. It was subsequently found that the patient had lost both dorsalis pedis and posterior tibial pulses. Occluding emboli was found distal to the operative site during endarterectomy; the patient suffered no vascular or neurologic deficit.
Of the eleven procedures monitored with both oxygen saturation and tibial SSEP's none had a significant change in the left or right tibial evoked response. The remaining four procedures monitored with both modalities had a rapid decrease followed by a complete loss in measurable oxygen saturation from the left great toe, representing 36%. In each procedure compression of the vascular structures was released with immediate return of measurable oxygen saturation and no postoperative deficit.
Conclusions: The data strongly suggests that pulse oximetry has a greater sensitivity for iliac artery compromise than SSEPs. The cases monitored with pulse oximetry showed a loss of signal before any significant change occurred in the SSEPs. Furthermore, based on our SSEP data, when the vascular structures are compromised it primarily affects the left leg.
TECHNICAL REVIEW
Anterior vs. Extreme Lateral Approach to the Lumbar Spine
Daniel Slepian, PA, CNIM
Anteror Lumbar Discectomy and Fusion
The anterior approach to lumbar spinal surgery has been widely used to treat degenerative pathology. This surgical procedure is routinely accomplished with the assistance of a vascular surgeon and entails an abdominal incision and manipulation of the viscera to expose the anterior lumbar spine. One complication associated with this procedure is occlusion of the iliac or femoral artery, either by an occluding emboli or a dislodged atherosclerotic plaque. This complication alone, if left undetected, may have signification consequences.
In our practice we incorporate standard pulse oximetery as an adjunct to tibial somatosensory evoked potentials. Our experience suggests that a considerable amount of time may lapse prior to the observation of a 10% change in the latency and or a 50% reduction in amplitude of the tibial SSEP. This time delay suggests that the somatosensory evoked potential is somewhat insensitive to ischemia.
Pulse oximetery, on the other hand, provides immediate feedback when an arterial occlusion occurs. A distinct advantage of the anterior approach, however, is the increased number of levels that can be addressed with this type of exposure, specifically L1-2, L2-3, L3-4, L4-5 and L5-S1. EMG muscle groups commonly used with this procedure are: the transverses abdominis, rectus femoris, vastus lateralis, tibialis anterior and gastrocnemius.
Xtreme Lateral (XLIF) Approach to the Lumbar Spine
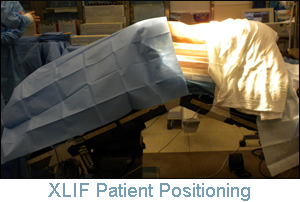 New techniques developed with the lateral approach to the lumbar spine have proven beneficial in reducing the morbidity associated with the anterior approach, but this technique also has associated complications. The levels that can be addressed include L1 through L5. Because of the iliac crest, L5-S1 cannot be addressed and sometimes L4-5.
New techniques developed with the lateral approach to the lumbar spine have proven beneficial in reducing the morbidity associated with the anterior approach, but this technique also has associated complications. The levels that can be addressed include L1 through L5. Because of the iliac crest, L5-S1 cannot be addressed and sometimes L4-5. 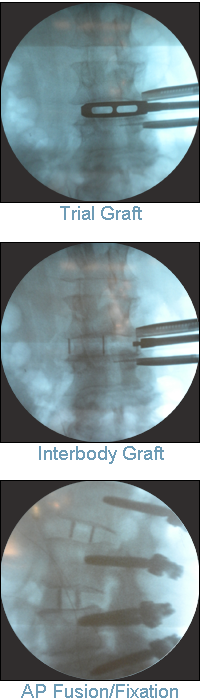 An advantage to this approach is that, depending on the number of levels, up to 4 small separate incisions are made to address each specific level. For example, with C-arm imaging, the probe is advanced through the psoas muscle. Because the roots of the lumbar plexus enter the muscle directly, it is necessary to monitor
multiple muscles for electromyographic activity.
An advantage to this approach is that, depending on the number of levels, up to 4 small separate incisions are made to address each specific level. For example, with C-arm imaging, the probe is advanced through the psoas muscle. Because the roots of the lumbar plexus enter the muscle directly, it is necessary to monitor
multiple muscles for electromyographic activity. The psoas muscle lies posterior and lateral to the abdominal aorta on the left side. The surgeon will need to pass through this muscle to accomplish the procedure. Emerging from the lateral border are the iliohypogastric, ilio-inguinal, lateral femoral cutaneous and femoral nerves. Emerging from the anterolateral surface is the genitofemoral nerve. This nerve supplies the cremaster muscle and scrotal skin. In the female it terminates in the skin of the mons pubis and labium majus.
Electromyographic activity from the L1 and L2 nerve roots can be monitored from a limited selection of muscles Including the cremaster muscle (L1, L2)and the transversus abdominis, which is innervated by the ventral rami of the lower six thoracic nerves and the first lumbar nerve. The vastus, lateralis, medialis and rectus femoris are innervated by L2, L3 and L4 respectively; the latter two nerves are primary. The other option is to place needles in the cremaster muscle, which could be very difficult to accurately identify. Additional EMG muscle groups may include the tibialis anterior, L4, L5 and the gastrocnemius, S1 and S2.
Although each procedure has related risks and complications, the lateral approach can accomplish in many cases what can be done by the abdominal approach to the lumbar spine. It is thus an excellent alternative to the anterior approach.
Reported complications (limited series)
1) Ipsilateral L4 nerve root injuries
2) Lateral femoral cutaneous nerve injuries
3) Thigh dysesthesia
4) Quadriceps weakness
These complications have also been reported with the open anterior approach. Complication Reference: North American Spine Society January 5th 2010
NEUROTECHNOLOGIST REFERENCE GUIDE
Third Edition
 You have your mind-set and equipment prepared for your 7:30 a.m. anterior cervical fusion. As you travel to the OR suite, you anticipate the modality sequence. The evoked potentials and EMGs to be monitored and electrode selection are ready, and so are you.
You have your mind-set and equipment prepared for your 7:30 a.m. anterior cervical fusion. As you travel to the OR suite, you anticipate the modality sequence. The evoked potentials and EMGs to be monitored and electrode selection are ready, and so are you.
When you check in with the charge nurse to verify your case, she says, "I have an anterior/posterior thoracolumbar procedure scheduled with the surgeon, not an ACF." A look of surprise crosses your face and you inquire again to verify the procedure. The charge nurse points to the schedule, looks up at you, shrugs her shoulders, and says, "Sorry, a thoracolumbar is scheduled." This isn't the first time a switch like this has happened and most likely will not be the last. It's a simple matter to deal with because you are well-versed in changing directions in midstream.
You take out your ORIMtec Neurotechnologist Reference Guide and simply refer to section 4's procedure-specific modality, turning to "Thoracic Procedures T2–T12." After reviewing the suggested modalities, you quickly shift your thought processes. Once your laptop fires up, you enter the new protocol. After referring to the guide again, you select the muscle groups and identify the needle insertion points. You are back on track and ready to go when the surgeon enters the OR 5 minutes early. This scenario highlights the value of using the Quanmtum Neuromonitoring Neurotechnologist Reference Guide as an adjunct to your existing skills, training, and experience.


